Researchers are developing technology that could one day “print” human skin on wounded soldiers and burn victims.
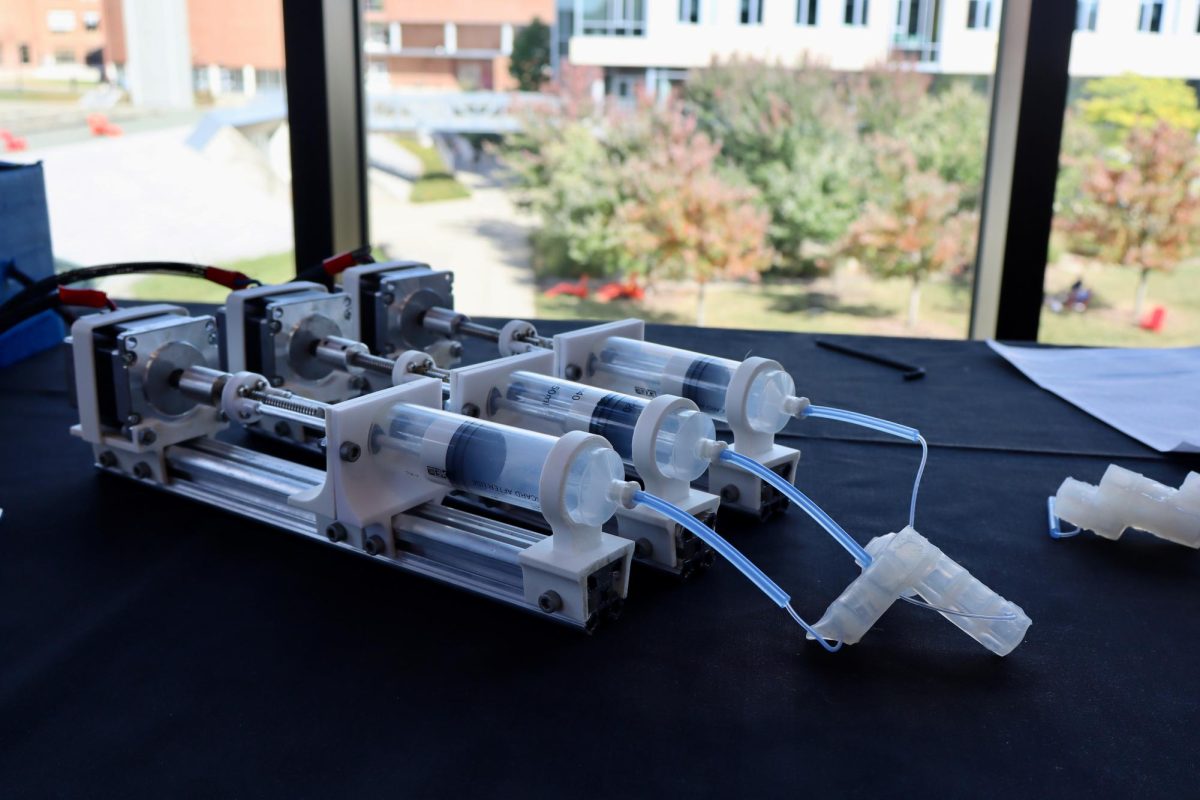
The technology was developed by modifying standard inkjet printers. Vials of the patients’ cells are substituted for ink cartridges and skin, and new layers of tissue are printed directly onto the affected area of a patient’s body.
The technology, developed at the Wake Forest Institute for Regenerative Medicine, will be funded over the next five years with $45 million from the Armed Forces Institute of Regenerative Medicine (AFIRM), a branch of the Department of Defense. The project has been in development for approximately three years.
The concept for biological skin printing has been around for years, but biotechnology has only recently become ready for the creation of functional tissues and organs.
Biological printing technology would be used to treat burns of varying degrees and damaged tissues of varying types while avoiding scarring altogether. Cells from the patients own body would be harvested and replicated in a specialized environment and prepared for spray on application to the affected area.
With the new technology, severe burns would be expected to heal within three weeks, according to Lt. Col. Brian Moore, Deputy Director of AFIRM.
“While this treatment will first be tested in burns, it’s possible that it could also be used to treat scarring from previous burns – by removing the scarred tissue and rebuilding skin,” said Karen Richardson, the senior communications manager at the Wake Forest Institute for Regenerative Medicine.
The technology could be used in scar reversion to treat debilitating instances where scar tissue restricts the range of motion near the joints or prevents the flexing of the feet and hands, according to Moore.
Biological skin printing also offers the ability to treat patients with severe burns over a large portion of their body.
“Current methods require grafting, which means to surgically remove a piece of healthy skin and transplant it to the burned area. This is not only very painful, but in some patients there is not enough unburned skin to harvest,” said Richardson.
Once the technology becomes affordable people who burn themselves cooking in the kitchen could have new skin printed directly onto their wound in a matter of hours, or could have their unwanted scars surgically removed and fresh flesh grown in its place.
Richardson added that this technology will be considered in treatment for skin ulcers and in patients with diabetes.
Moore explained that similar technology is already being used to repair heart and bladder tissues.
The first step in the process involves taking a stamp sized skin sample from the patient, isolating cells, and replicating them in a specialized environment.
Pluripotent stem cells, cells capable of differentiating into nearly all cell types, would ideally be isolated and transformed into cultures of specialized cell types, according to Moore.
The next step involves scanning the wound to determine its size and depth. From this scan, an automated program reconstructs a 3D model or “map” of the damaged or missing skin – so that the printer can apply the correct type and number of cells for re-growth, Richardson explained.
“Different types of cells are placed in vials – along with a gelatin-like material that helps the cells adhere to the wound. All are ‘printed’ directly onto the wound,” said Richardson.
“In animal studies, mice with wounds similar to burn wounds healed in three weeks with bioprinting. In animals without the treatment, wound healing took five weeks,” Richardson added.
Testing of the technology, which is currently in the pre-clinical phase, has been limited to mice, but researchers hope to begin testing on larger subjects such as pigs soon, said Moore.
“The goal of the project is to develop a treatment that can quickly cover and stabilize a wound. Research has shown that the longer it takes to cover a wound with skin, the higher the risk of infection, complications and death,” Richardson said.
Human clinical testing is still approximately five years away and Moore predicts that a Food and Drug Administration licensure will follow three to five years after that.
Moore thinks there will be a big civilian market for the technology and described the investment as “high-risk [and] high-benefit.” He added that the project currently has garnered the support of Lexmark, a company that manufactures printers, and hopes to continue to get industry interested in the project.
Once licensed, the technology will simultaneously be made available to the military and public.
Brian Canova can be reached at [email protected].